Understanding Pelvic Floor Physiotherapy for Prolapse
What is Pelvic Floor Physiotherapy?
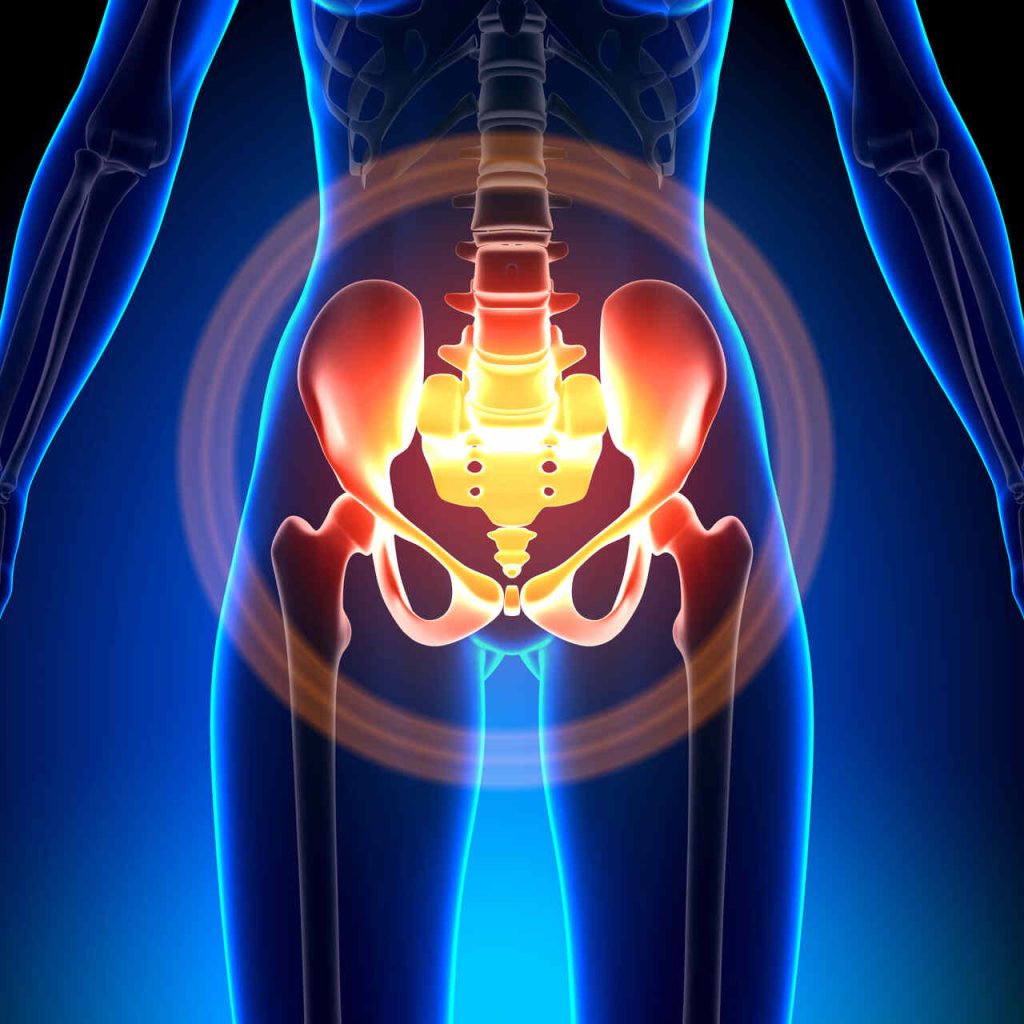
Pelvic floor physiotherapy is a specialized form of physical therapy aimed at addressing issues related to the pelvic floor muscles. These muscles play a crucial role in supporting pelvic organs such as the bladder, intestines, and uterus. They also aid in bowel and bladder control and sexual function.
In the context of prolapse, pelvic floor physiotherapy focuses on strengthening and rehabilitating the muscles to alleviate symptoms and improve quality of life. This type of therapy involves targeted exercises, manual techniques, and education on lifestyle modifications. It is an effective, non-surgical option for managing prolapse symptoms and enhancing overall pelvic health.
For those seeking more information on what a session might involve, check out our detailed guide on pelvic floor physiotherapy treatment.
How Does Prolapse Affect the Pelvic Floor?
Pelvic organ prolapse occurs when the muscles and tissues supporting the pelvic organs weaken, causing one or more of the pelvic organs to descend into or outside the vaginal canal. This condition commonly affects women, particularly those who have given birth, undergone pelvic surgery, or are experiencing menopause.
Common Impacts of Prolapse on Pelvic Floor:
- Pelvic Pressure: A feeling of heaviness or fullness in the pelvic area.
- Discomfort: Pain during intercourse or while performing daily activities.
- Bladder Issues: Difficulty emptying the bladder, frequent urination, or stress incontinence.
- Bowel Changes: Constipation or a sensation of incomplete bowel evacuation.
The table below illustrates the typical symptoms experienced in different types of prolapse:
| Type of Prolapse | Common Symptoms |
|---|---|
| Cystocele (Bladder) | Urinary incontinence, urgency, frequency |
| Rectocele (Rectum) | Difficulty with bowel movements, rectal pressure |
| Uterine Prolapse (Uterus) | Pelvic pressure, pain during intercourse |
| Enterocele (Small Intestine) | Lower back pain, pelvic discomfort |
Understanding how prolapse affects the pelvic floor muscles is crucial for effective treatment. Through a comprehensive evaluation, a pelvic floor physiotherapist can identify the specific areas of weakness and create a personalized treatment plan. For more insights on how prolapse impacts daily life and other related conditions, you can read our articles on pelvic floor physiotherapy for urinary urgency and pelvic floor physiotherapy for pregnancy.
For further details on recognizing the symptoms of pelvic floor disorders, please visit our section on Recognizing Pelvic Floor Disorders.
Signs and Symptoms of Pelvic Prolapse
Pelvic prolapse occurs when the muscles and tissues supporting the pelvic organs weaken, causing one or more of the pelvic organs to descend or press into or out of the vaginal canal. Recognizing the signs and understanding the impact on daily life can aid in seeking timely treatment.
Recognizing Pelvic Floor Disorders
Identifying pelvic floor disorders early can significantly improve treatment outcomes. Here are some common signs and symptoms associated with pelvic prolapse:
- A Sensation of Heaviness or Pressure: Many individuals experience a feeling of heaviness or pressure in the pelvic area, often described as a dragging sensation.
- Visible Bulge: In some cases, a noticeable bulge may be seen or felt coming out of the vaginal canal.
- Difficulty with Bowel Movements: Problems with bowel movements, including constipation or a sensation of incomplete evacuation, can be indicators of pelvic floor disorders.
- Urinary Issues: Symptoms such as urinary incontinence, urgency, or a frequent need to urinate may occur.
- Sexual Discomfort: Discomfort or pain during sexual activity can be a sign of pelvic floor dysfunction.
| Symptom | Frequency (% of Affected Individuals) |
|---|---|
| Heaviness or Pressure | 85% |
| Visible Bulge | 60% |
| Bowel Movement Issues | 55% |
| Urinary Problems | 70% |
| Sexual Discomfort | 50% |
Understanding the Impact on Daily Life
Pelvic floor disorders can affect various aspects of daily life. Here’s how they might impact day-to-day activities:
Mobility and Activities
The feeling of pressure or a visible bulge may discourage individuals from participating in physical activities, impacting mobility and overall quality of life. Activities like walking, lifting, or exercising can be limited due to discomfort or fear of worsening symptoms.
Emotional Well-being
The symptoms of pelvic prolapse can lead to emotional distress, impacting mental health. Feelings of embarrassment, frustration, or anxiety are common, as individuals may feel self-conscious about their condition. For more information, refer to our section on when to see a pelvic floor physiotherapist.
Relationships and Sexual Health
Sexual discomfort is a significant concern for many experiencing pelvic prolapse. This can strain intimate relationships and negatively impact sexual health. Learn more about addressing these concerns in our article on pelvic floor physiotherapy for sexual health.
Addressing these symptoms through pelvic floor physiotherapy for prolapse can significantly improve quality of life. By recognizing the signs and understanding the impact, individuals can seek appropriate treatment and embark on a journey towards better health.
Benefits of Pelvic Floor Physiotherapy
Strengthening the Pelvic Muscles
Pelvic floor physiotherapy for prolapse aims to strengthen the pelvic muscles, offering core stability and essential support for the organs located in the lower abdomen. More robust pelvic muscles can alleviate the symptoms of prolapse and boost overall pelvic health. A stronger pelvic floor helps prevent the progression of prolapse and mitigates the risk of other pelvic floor disorders.
| Benefit | Description |
|---|---|
| Increased Muscular Strength | Enhances the ability to support pelvic organs |
| Prevention of Prolapse Progression | Reduces the likelihood of prolapse worsening over time |
| Enhanced Core Stability | Contributes to better overall posture and balance |
For more information on specific exercises, explore our comprehensive guide on pelvic floor exercises.
Improving Pelvic Floor Function
Improving pelvic floor function is another significant benefit of physiotherapy. Enhanced function leads to better bladder and bowel control, minimizes pelvic pain, and can significantly enhance one’s quality of life. Effective pelvic floor exercises can help individuals regain control over their bladder and bowels, alleviating symptoms tied to incontinence and constipation.
| Aspect | Improvement |
|---|---|
| Bladder Control | Reduces incidents of urinary leakage |
| Bowel Control | Minimizes occurrences of constipation and bowel incontinence |
| Pain Reduction | Alleviates pelvic pain, making daily activities more manageable |
To find a specialist for tailored treatment plans, visit pelvic floor physiotherapy near me.
Addressing Prolapse Symptoms
Pelvic floor physiotherapy is essential for addressing prolapse symptoms. This includes reducing the feeling of heaviness or bulging in the pelvic area and lowering discomfort or pain during physical activities. Specific exercises and techniques can significantly lessen the severity of these symptoms, leading to a better quality of life.
| Symptom | Relief |
|---|---|
| Heaviness or Bulging | Reduces the sensation in the pelvic region |
| Discomfort/Pain | Lowers pain levels during daily activities |
| Urinary Issues | Decreases urinary urgency and frequency |
For further reading on how treatment can help with incontinence issues, refer to pelvic floor physiotherapy for incontinence.
Pelvic floor physiotherapy offers numerous benefits for managing and alleviating the symptoms of prolapse. With the right treatment plan, you can significantly improve your pelvic health and overall well-being.
The Role of a Pelvic Floor Physiotherapist
A pelvic floor physiotherapist plays a crucial role in addressing the issues related to pelvic organ prolapse. They are trained to help individuals improve their quality of life through specific assessment and personalized treatment plans.
Evaluation and Assessment
When I first visit a pelvic floor physiotherapist, they conduct a thorough evaluation and assessment to understand my specific needs and challenges. This process is essential for developing an effective treatment plan tailored to my condition. The assessment typically involves:
- Medical history: Understanding any previous health issues, surgeries, or conditions that could affect my pelvic floor.
- Physical examination: Assessing the strength, coordination, and functionality of my pelvic floor muscles.
- Symptoms review: Discussing my symptoms, their severity, and how they impact my daily life and activities.
| Assessment Areas | Details |
|---|---|
| Medical History | Past surgeries, childbirth, existing health conditions |
| Physical Examination | Muscle strength, functionality, coordination |
| Symptoms Review | Severity, impact on daily activities |
These evaluations help the physiotherapist to pinpoint the areas of concern and determine the best course of action for my specific prolapse issues. For more on when to seek a pelvic floor physiotherapist, check out when to see a pelvic floor physiotherapist.
Individualized Treatment Plans
Following the evaluation, the physiotherapist creates an individualized treatment plan to address my unique needs. This plan typically includes a range of techniques and exercises designed to strengthen my pelvic floor muscles and alleviate the symptoms of prolapse.
Key components of an individualized treatment plan:
- Pelvic Floor Exercises: Essential exercises to build strength and improve muscle control. For more details, see pelvic floor exercises.
- Postural Correction: Techniques to enhance my posture, reducing strain on my pelvic floor.
- Lifestyle Modifications: Suggestions to alter daily habits that may be affecting my pelvic health.
Each plan is customized to suit my specific condition and progress. The physiotherapist may also adjust the plan as I improve, ensuring that it continues to meet my needs and helps me achieve my health goals.
| Treatment Component | Purpose |
|---|---|
| Pelvic Floor Exercises | Strengthen muscles, increase control |
| Postural Correction | Reduce strain, improve alignment |
| Lifestyle Modifications | Support overall pelvic health |
Regular sessions with a pelvic floor physiotherapist ensure that I receive continual support and guidance. For more information on the benefits of this treatment, check out benefits of pelvic floor physiotherapy. Understanding and following my individualized treatment plan can significantly enhance my journey towards better pelvic health.
Exercises and Techniques
Engaging in pelvic floor physiotherapy for prolapse involves various exercises and techniques that can significantly improve pelvic health and alleviate symptoms. Here, I’ll explore different methods to strengthen, support, and enhance pelvic floor function through targeted exercises, postural adjustments, and lifestyle changes.
Pelvic Floor Strengthening Exercises
Pelvic floor strengthening exercises are designed to fortify the muscles that support the bladder, uterus, and rectum. Performing these exercises consistently can lead to significant improvements in pelvic strength and function.
Common Pelvic Floor Exercises:
- Kegels: Focus on tightening and holding the pelvic muscles for a few seconds, then releasing. Repeat multiple times.
- Bridge Pose: Lie on your back with your knees bent, lift your hips towards the ceiling, and engage your pelvic muscles.
- Squats: Perform squats while concentrating on engaging and lifting the pelvic floor muscles.
For a comprehensive guide on these exercises, visit our article on pelvic floor exercises.
Postural Correction Techniques
Proper posture plays a crucial role in reducing stress on the pelvic floor. Implementing postural correction techniques can enhance the effectiveness of pelvic floor physiotherapy.
Tips for Postural Correction:
- Neutral Pelvic Alignment: Maintain a straight spine and neutral pelvis while sitting, standing, or walking.
- Pelvic Tilts: Perform gentle tilting of the pelvis to promote flexibility and strength.
- Ergonomic Adjustments: Ensure that workspaces are set up to encourage good posture.
These techniques, when practiced regularly, can significantly reduce the strain on the pelvic floor and aid in the management of prolapse symptoms.
Lifestyle Modifications
Incorporating specific lifestyle changes can further enhance the benefits of pelvic floor physiotherapy. These modifications are essential for maintaining pelvic health and preventing the exacerbation of prolapse symptoms.
Suggested Lifestyle Changes:
- Healthy Diet: Consume a balanced diet rich in fiber to prevent constipation and reduce pelvic pressure.
- Hydration: Maintain proper hydration to support overall health and minimize urinary urgency.
- Regular Exercise: Engage in low-impact exercises such as swimming, walking, or yoga to stay active without straining the pelvic floor.
Implementing these lifestyle modifications alongside your physiotherapy routine can provide comprehensive support for pelvic health.
For more detailed information on specific treatments, visit our articles on pelvic floor physiotherapy for constipation and pelvic floor physiotherapy for pelvic pain.
By incorporating these exercises, postural corrections, and lifestyle modifications, I can take proactive steps towards empowering my journey through pelvic floor physiotherapy for prolapse.
Empowering Your Journey with Pelvic Floor Physiotherapy
Setting Realistic Goals
When embarking on a journey with pelvic floor physiotherapy for prolapse, it’s essential to set achievable, realistic goals. I need to understand that progress might be gradual, and having incremental milestones can help keep me motivated. Here are some key factors in goal-setting:
- Assessment Results: My initial evaluation by a pelvic floor physiotherapist will provide a baseline.
- Prioritizing Symptoms: Focus on alleviating the most debilitating symptoms first.
- Functional Improvements: Aim for improvements in daily activities.
Committing to Consistency
Consistency is key in strengthening the pelvic floor and managing prolapse symptoms effectively. I need to incorporate the recommended exercises and routines into my daily schedule. Here’s how I can stay committed:
- Scheduled Sessions: Set specific times for pelvic floor exercises.
- Routine Integration: Integrate exercises into my daily routine, such as practicing them while watching TV or before bedtime.
- Tracking Progress: Maintain a log to track my exercise habits and improvements.
Table: Weekly Exercise Tracking
| Day | Exercise Completed | Notes |
|---|---|---|
| Monday | Yes | Felt improvement |
| Tuesday | Yes | Mild discomfort |
| Wednesday | Yes | Increased stamina |
| Thursday | Yes | No issues |
| Friday | Yes | |
| Saturday | Rest | |
| Sunday | Yes | Great session |
Monitoring Progress
Regularly monitoring progress helps me stay informed about my improvements and adjust the treatment plan if needed. Here are ways to effectively keep track:
- Regular Assessments: Schedule follow-up appointments with my physiotherapist to evaluate progress.
- Symptom Diaries: Maintain a diary to document changes in symptoms and any new concerns.
- Adjustments to Plan: Based on my progress, my physiotherapist might suggest modifications to my treatment plan.
By setting realistic goals, staying consistent, and closely monitoring my progress, I can effectively manage my pelvic floor health. To learn more about various techniques and benefits, visit our articles on pelvic floor exercises and benefits of pelvic floor physiotherapy.